Whitepaper
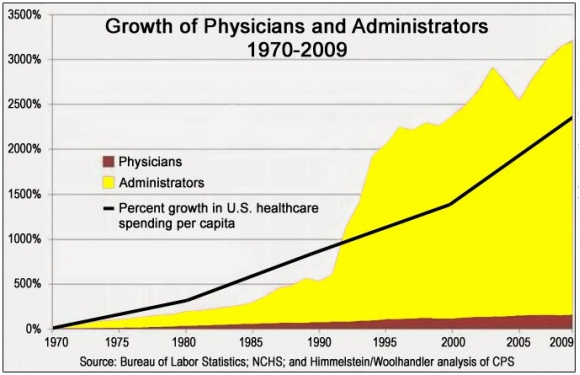
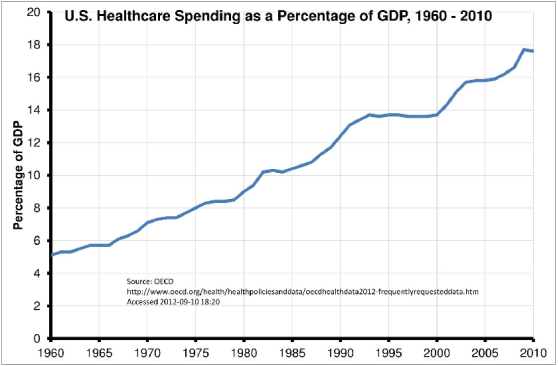
A significant portion of healthcare costs are caused by wasteful management of patient health data, and perpetuated by industries that capitalize on this wastefulness. The United States' 10-to-1 ratio of administrators to doctors tells the whole story. [1]
Healthchain was born of two professionals from Stanford: a psychiatrist and a software engineer. We realized two important things:
-
Most of the unnecessary costs of healthcare are systemic, even within esteemed institutions like Stanford.
-
They cannot be circumvented even by founding our own company (we tried).
Healthchain enables you to carry your health data on your cell phone. You can share this data with any new doctor, as easily as sending an email, and avoid repeating diagnostic tests -- even in a foreign country. Upload prescriptions to Healthchain, and let pharmacies bid to fill your prescriptions at the lowest price. Make passive income when researchers offer you money to share your health data anonymously.
This is only the beginning, and it begins now.
Hospitals charge patients a small fee to access their records. The retrieval process takes time, and requires paperwork from both patients and administrators. These barriers make patients feel helpless. If patients are finally granted access to their data, they are usually only given access to limited data. EPIC is the most commonly used electronic medical record (EMR) software in the US, used by 54% of the population and many university hospitals. EPIC promises interconnectivity, but in the experience of Healthchain founders, it fails to deliver for either patients or doctors.
Health data is of primary concern to patients, and patients do not have custody of their own health data. They cannot easily share their data with new medical service providers or seek a second opinion from a doctor from a different hospital. This introduces new costs to all parties, as it requires patients to pay for new tests, doctors to perform them, administrators to record them, and insurance companies to cover all of the preceding.
No single point of contact exists for all of a patient’s health data.
Within an industry dedicated to improving patient health, the refusal to share information in pursuit of that purpose runs to the core business model of most medical service providers and insurance companies. Rather than working together to fulfill and minimize the necessity of healthcare, market participants compete to obstruct one another's competence by controlling information.
"The fundamental driver of most behavior in healthcare is the reimbursement scheme," writes Dave Chase, former head of Microsoft Health.
While we might prefer to live in a world where everyone acts in harmony to fulfill a common goal like healthcare, the reality is we all need dinner on the table and a place to sleep and charge our cars. Thus, behavior patterns follow incentive patterns, no matter how absurd or counter-productive they may become through history, lack of technology, habit, and policy.
For example, most medical service providers (MSPs) are paid to provide health services, establishing a strange conflict of interest between provider revenue and long-term, society-wide healing. A healthier population requires fewer health services. Pharmaceutical companies face the same conflict -- a pill that costs $100 million to develop and cures disease in a single dose might be a human victory, but a stockholder calamity.
Healthchain anticipates incentive structures and provides a platform to create new ones that align with the true goals of healthcare. This reduces overhead costs for various market participants, making plain the business case for adoption. Where incentive structures may currently reward delays, repetitions, and other outcomes that don't best benefit the patient, Healthchain satisfies the need to rearrange and circumvent them.
-
Duplication - Every medical service provider and insurance company maintains its own database. Much of this data is duplicated, giving rise to the claim-filing industry.
-
Centralization - To reduce the costs and difficulty of maintaining centralized databases, both providers and patients are incentivized toward centralization. Doctors may prefer to run their own practice, but without experience maintaining complex databases, they are left with little choice but to join a large hospital. Patients may want to see a new doctor at Hospital B, but since his records are already held at Hopsital A, he decides to find a new doctor at Hospital A instead. These supply- and demand-side centralization forces result in the unnatural growth of medical organizations, making healthcare more corporate and less personal.
-
Isolation - Health care data is isolated by the boundaries of the organization in which it is stored. Thus, researchers only have access to partial data for each patient.
-
Unnecessary middlemen - For example, pharmacy benefit managers (PBMs) profit from fragmentation of data by coordinating between insurance companies, pharmacies, and drug manufacturers:
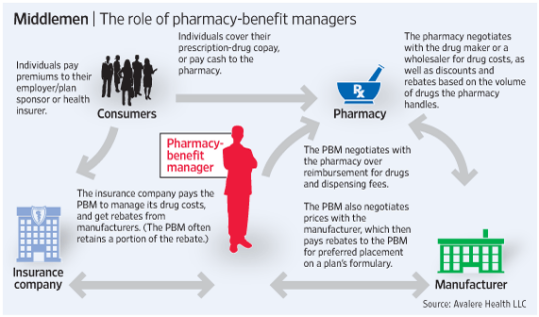
While PBMs may seem well-positioned to bring savings to customers, their lack of transparency often results in profiteering at cost to the consumer.
- Increased administrative costs - These core problems result in soaring administrative costs, as a percentage of total healthcare costs:
When the foundations for today's systems were laid, we did not have the technology to maintain an immutable database without a central organization. The innovations presented in the Bitcoin paper[a] and the subsequent success of the Bitcoin network prove that we can now run a decentralized, trustless database for value storage, communication, and computation.
Now that we have the technology we need, we must address the incentive structures underlying the current healthcare industry.
Phase 1: Patients find the perfect doctor using AI matching software (already built); Doctors attract new patients
-
To encourage network growth, Phase 1 helps patients find the perfect doctor using our AI matching software. When patients add their health data, our software uses it to match them with the best doctor or healthcare provider for their case. The right doctor, especially in a mental health setting, can have a tenfold impact on the treatment outcome.
-
Patient health data is stored on IPFS and secured with public-key encryption, allowing patients to share health data easily with any new doctor and avoid repeating diagnostic tests. Public-key encryption ensures patient data cannot be read or accessed by anyone, including Healthchain. A hash of the data is stored on the blockchain. We have already created the software for this.
-
Doctors attract new patients, and have access to their complete, structured health data
-
Doctors gain free access to Healthchain’s AI-powered electronic medical record (EMR) software (optional), developed over 3 years with input from 15 doctors. Patient data added to the EMR is automatically uploaded to Healthchain. We have already created the software for this.
-
Patients receive Health tokens when they sign up, add health data, and book appointments.
Phase 2: Pharmacies bid to fill prescriptions, increasing profit margins while reducing cost to patients.
-
Doctors upload prescriptions to Healthchain, and pharmacies search for prescriptions by zip code. The medication and amount prescribed is shown, but the patient’s name and address are only revealed upon acceptance of a bid. We have already created the software for this.
-
Pharmacies access the network and place bids for free, and pay a small fee (0.01 HLT) for each accepted bid. This drastically increases pharmacy profit margins.
-
To prevent prescriptions from being filled multiple times, pharmacies add filled prescriptions to a revocation list stored on the blockchain.
Phase 3: EMR integration with Healthchain allows doctors using other records systems to export and add health data to Healthchain.
-
At this stage, EMR software companies will face market pressure from patients and doctors and will integrate with Healthchain.
-
Data from other EMRs can be used to strengthen validation of patient and doctor identities.
Phase 4: Researchers pay patients for anonymous health data for use in clinical studies, creating a streamlined health data marketplace and a source of passive income for every patient.
- Researchers can specify a precise budget and patient criteria and find qualifying patients in hours or days, instead of months.
- Healthchain becomes the primary infrastructure for the multibillion-dollar health data industry.
- American prices for data create a significant source of income for families in developing economies, increasing network effects internationally and creating a global research market, improving research.
Why do we need decentralization? Decentralized systems run slower and cost more to develop and maintain than centralized systems.
Microsoft Health Vault, Google Health, and others have tried creating centralized health data custody systems -- and failed. Patients are reluctant to trust centralized systems with their health data. Employers can deny jobs due to health conditions, and insurance companies can raise premiums. Centralized databases can also be used for data mining and advertising, and can expose millions of records in a single security breach.
Healthchain's public-key encryption ensures nobody can read patient data, except for the patient and designated providers. Not even Healthchain's software team can access patient data, nor use it for any purpose, without patient consent.
Decentralized health records thus overcome some of the fatal flaws of centralized data custody systems. In addition, a decentralized health network also allows us to accomplish the following:
Patient custody allows the sharing of health data across organizational boundaries, dramatically increasing transparency and efficiency while maintaining privacy. It also gives patients a unified picture of their health data, the opportunity to earn money from the value of their health data, and reduced medication costs through pharmacy bidding.
With all health data stored on a decentralized, tamper-proof database, patients can easily give insurance companies access to their health data and allow them to compete for their choice of insurance policy. This enables lead to peer-to-peer insurance exchanges, where individuals can bid to insure one another.
A new graduate does not need to run a central EHR system. Since the data is now decentralized, she can see the complete medical data of each patient.
Without the burden of database management, new doctors can run a more personal private clinic with less administration.
Once your prescription is on Healthchain, pharmacies compete to offer you the best price for your medications, which are then shipped to your door. Lack of patient custody is the only obstacle to this reality.
When health data is stored in a blockchain database, a clinic is able to bill two patients from two different insurance companies seeing the same provider at the same time.
A researcher from Stanford can pay health tokens to every cancer patient who makes available their medical records for a new study. The patients interested can simply add the public key of Stanford University, and their medical data immediately becomes available to the researcher.
With Healthchain, patients can seek a second opinion by adding the public key of another doctor to their health records.
Clinicians can access more structured and correlated data instead of just reams of PDF files and paper-based notes. This helps to inform better decision-making and improve patient care.
By keeping all patient data in the same place, doctors have access to graphs and long-term patterns in health data, such as allergies and medications, that will improve their ability to treat patients appropriately.
Labs often refuse to integrate with small private practices. With Healthchain, health data will be decentralized and standardized, making integration easy.
Developing economies can avoid the infrastructure problems and inefficiencies created by more advanced economies before blockchain technology became available.
Patients become able to participate in a community of others with similar health profiles.
Records that prevent fraud, like revocation lists for patient prescriptions, can be secured using blockchain technology.
Note: For a centralized example, see ELGA in Austria [2].
Patients have access to a wealth of health apps, but not the data that would make them valuable. Only the most motivated patients retrieve their health data from centralized databases and make use of it in an app. A blood-sugar tracker or a weight-loss app is far more useful when patients can access their data from a secure healthcare record and feed it directly into the app. Patients become empowered and responsible for their own healthcare.
If patients becomes ill while traveling, they can instantly access their records and share them with a doctor abroad.
By issuing health tokens as the unit of accounting for internal transactions, Healthchain participants can "defibrillate" the healthcare industry out of inertia by creating new, efficient marketplaces where none had existed before. This allows Healthchain to transform incentive structures industry-wide and offer current market participants new opportunities to profit.
Tokenization enables the following:
The value of health tokens is backed by the business they create: protocol development, and the exchange of data between healthchain entities.
The average retail pharmacy’s profit margin is around 12%, as most profit is captured by PBMs. (source)
Tokenization allows Healthchain to reward early adopters who join the network and make it valuable for other market participants.
An accounting system that reflects each person's contribution is essential for inspiring participation in the Healthchain community.
Healthchain creates a market with patients in control of their data on the supply side and researchers who want access to the data on the demand side.
Tokens allow Healthchain to autonomously reward desired behaviors in order to mitigate prescription non-compliance and lifestyle diseases, each of which is responsible for a significant portion of healthcare costs.
Tokens not sold are held by the Healthchain Foundation, which allows token holders to submit and vote on smart-contract proposals for fund allocation.
Uses
- Find the perfect doctor with AI-powered matching software
- Schedule doctor appointments instantly
- Upload, access, and share all health data for free
- Control permissions for their health data
- Share data easily with any medical service provider
- Keep data private and secure
- Write wearable data to Healthchain
- Receive paid offers from researchers to access de-identified health data
- Search network of medical service providers to find doctors on Healthchain
- Book appointments with medical service providers at a discount
Benefits
- Find the best doctor for them, instantly
- Avoid repeated diagnostic tests
- Reduce medication costs
- Earn passive income
- Earn active income
- Avoid data mining and advertising based on health data
- Improve diagnoses and treatment outcomes
Uses
- Join Healthchain network to be discovered by patients
- Use Healthchain’s state-of-the-art EMR with rapid calendaring and artificial intelligence
- Access total patient health history
- Graph patient history to improve treatment plans
- Send prescriptions to Healthchain
Benefits
- Acquisition of new patients
- Reduced burden of database management
- Reduced administrative costs
- Reduced software costs
- Improved patient outcomes
- Reduced liability
Uses
- Search nearby prescriptions
- Bid on prescriptions for free
- Pay 1 HealthBit (0.01 Health tokens) to Healthchain Foundation for each accepted bid
Benefits
- Increased profit margins
- Reduced PBM overhead
- Acquisition of new customers
Uses
- Specify a budget for each study
- Pay 90% of budget to participating patients
- Pay 10% to the Healthchain Foundation
- Quickly find qualifying patients
- Obtain complete patient health data from one source
Benefits
- Streamlined data collection process
- Reduced wait times
- Accurate budgeting
Uses
- Offer lower premiums to patients directly
Benefits
- Reduced payouts due to repeated diagnostic tests
- Reduced payouts due to high medication costs and PBM overhead
- Reduced payouts due to medical service provider administrative costs
- Reduced payouts due to lifestyle disease
- Reduced payouts due to prescription non-compliance
- Reduced payouts due to ineffective treatment caused by lack of access to health data
- Reduced payouts due to insurance fraud
- Reduced payouts due to malpractice
A large network incentivizes market participants to adopt healthchain as industry protocol. Therefore, end users are enabled join the network as easily as possible.
Only entities that immediately and directly profit from access to the network pay a fee. For example, if five pharmacies place bids to fill one prescription, only the winning pharmacy pays a fee. This arrangement encourages more pharmacies to bid on patient prescriptions and begin to profit from Healthchain right away.
Pharmacies and researchers have different transaction costs because for pharmacies, the value comes from access to the database but not from the data itself. For researchers, the value comes from the data itself.
Advertisements are not allowed on the network. We believe health decisions should be based only on the efficacy of a treatment and its appropriateness for each patient, and not on an entity’s ability to advertise.
IPFS
Blockchain
Ethereum smart contracts
PKI - Public-key encryption (PKI) is an encryption method that has never been broken in the 20 years since its inception. Any information encrypted with a public key can only be de-encrypted with a private key. This means the only person who can de-encrypt the data is the patient. It would take a hacker so long to break this encryption that the sun would burn out before they succeeded.
Healthchain's Electronic Medical Record (EMR) software was developed over 3 years with continual input from 15 doctors at Savant Care in Los Altos, CA. The EMR is guided by artificial intelligence and features a conversational user interface.
Developed by doctors, for doctors
Developed over three years with continual input from Savant Care’s 15 doctors in Los Altos, CA.
Fastest on the market
Doctors are enabled to schedule appointments and edit patient data about ten times faster than with other leading EMR software.
Virtually free to use
Savant Care’s EMR has been compared to another service that costs $300 per month. Healthchain will be free for the first year, and cost only 1 health token per month after that. This saves doctors hundreds of dollars per month in costs on EMR software alone.
Uses IPFS for storage
The Healthchain EMR uses the decentralized IPFS for storage, eliminating storage costs for Healthchain and its users while maintaining transaction speed.
Beloved by doctors
Healthchain’s EMR has been enjoyed for years by the doctors at Savant Care. Many doctors from other organizations have requested that Savant Care make their EMR available for sale -- the calendar function alone was highly requested. Healthchain makes the entire EMR fully available to any doctor, at virtually no cost.
Screenshots
- Principal accounting unit for all internal transactions
- Grants token holder permission to submit proposals to the Healthchain Foundation
- Grants token holder permission to vote on proposals submitted to the Healthchain Foundation
- Enables rewards based on user actions (active work)
- Grants users value based on sharing/disclosing data (passive work)
- Allows users to purchase services and products within Healthchain ecosystem (e.g., Doctors purchasing EMR software for 1 HLT/month)
- Allows users to sell services and products within Healthchain ecosystem (e.g., Pharmacies bidding to fulfill prescriptions)
- Provides incentive to new users to encourage product trial and usage
Token holders do NOT:
- Receive a share of Healthchain profits
- Receive rights associated with formal ownership of Healthchain
- Gain ability to participate in governance outside of Healthchain Foundation proposals and voting contracts
We cannot possibly anticipate all of the needs and market structures that will shape the healthcare industry of the future.
Therefore, we are establishing the Healthchain Foundation, which will use health tokens to incentivize market participants. The Foundation will also use tokens to fund software development, pay for storage on the Filecoin network, and cover other maintenance needs.
The Healthchain foundation will also be responsible for projects like the following:
-
Raising required capital
-
Academic research through grants
-
Community-building
The Healthchain Foundation is run through an Ethereum smart contract system. Any token holder can make a proposal in the form of an Ethereum transaction to send Ether or to execute a contract, and other token holders can vote for or against the proposal. We chose this structure because we believe the network will collectively have more intelligence than any committee.
Once tokens are created, the only way they can leave the Healthchain Foundation is via a successful voting contract. This protects token holders from theft and misappropriation of funds.
Requirements for proposals
- Minimum quorum for proposals: 10% of total tokens - This is the minimum amount of votes a proposal needs before it can be executed.
- Minutes for debate: 30 days - This is the minimum amount of time that must pass before a proposal can be executed.
- Margin of votes for majority: Over 50% of the votes
- Token holders can delegate their voting rights to other token holders on the network.
Incentive engineering
One of the primary goals of the Healthchain Foundation is to rearrange the incentive structures of industries whose profitability will wane in concordance with Healthchain's adoption. For example, PBMs are a trillion-dollar industry, and we cannot expect them to go quietly into the good night. Some ideas for a new incentive structure include the following:
- Giving PBMs health tokens to purchase mining rigs to maintain the Healthchain network
The Healthchain network is invited to participate in finding the most satisfying solution, perhaps even in discussion with PBM industry representatives, through the Healthchain Foundation and its proposal system.
Healthchain never sees patient data, as it is stored on the InterPlanetary File System (IPFS), a protocol designed to create a permanent and decentralized method of storing and sharing files. These files can only accessed by the patient’s secure private key.
The The Health Insurance Portability and Accountability Act (HIPAA) legislation is on our side. (Dr. S - elaborate?)
Our team previously founded Savant Care, an outpatient psychiatry practice in Palo Alto that also conducts research and development of machine learning algorithms, neural networks, and artificial intelligence for use in tracking and predicting mental health issues. We also created a complete Electronic Medical Record (EMR) software that features a conversational UI.
Dr. Savant has just released the world's first personal health record software that uses IPFS for storage and the blockchain to guarantee immutability and ordering of the data.
Dr. Vidushi Savant, MD -- Clinical Faculty, Stanford University Hospital; Co-Founder and Chief Medical Officer of Savant Care
Dr. Vidushi Savant, MD is a Stanford-trained psychiatrist, Chief Medical Officer and Co-founder of Savant Care, and a Clinical Faculty member at Stanford University. She is double board-certified in General Psychiatry and Psychosomatic Medicine. She received her Psychosomatic Medicine subspecialty training at Stanford Hospital, and completed her residency training in Adult Psychiatry at Loyola University Medical Center in Chicago, Illinois. She received her medical school education from Government Medical College in Patiala, India.
Dr. Savant has conducted intensive research and development of machine learning algorithms, neural networks, and artificial intelligence for use in tracking and predicting behavioral health issues, which she has deployed at Savant Care.
She received numerous achievement awards in research and certificates of appreciation for clinical work from the Department of Psychiatry at Loyola University Medical Center. She was nominated and inducted as a member Medical Honor Society Alpha Omega Alpha during her residency by the caucus of student members of the society based on her values of leadership, character, community service, and professionalism. She remained actively involved in medical student and resident teaching throughout her residency and fellowship at Stanford.
Affiliations & Accolades:
-
Psychosomatic Medicine Fellowship, Stanford Hospital
-
Clinical Faculty, Stanford University
-
Board-certified in General Psychiatry, American Board of Psychiatry and Neurology
-
Board-certified in Psychosomatic Medicine, American Board of Psychiatry and Neurology
-
Awards and certificates for excellence in psychiatry, Department of Psychiatry at Loyola University Medical Center
-
Member, Medical Honor Society Alpha Omega Alpha
Dr. Sonia Parikh, MD is an adult psychiatrist and chief medical advisor at Savant Care, Inc. She is the recipient of the Best of Los Altos Award for Psychiatrist (2015 & 2016), which is awarded by the city of Los Altos to one psychiatrist per year for excellence and service to the community.
She completed her residency training at Stanford Hospital and Clinics, where she gained expertise in treating the entire spectrum of mental illness through an integrative approach to psychological well-being — medications, psychotherapy and alternative treatments. After residency, she completed a fellowship in psychoanalytic psychotherapy through the San Francisco Center for Psychoanalysis. She attended UC San Diego School of Medicine for medical school, where she graduated with honors and was heavily involved in community outreach and increasing awareness for mental health issues. She obtained her bachelor’s degree from Cornell University, where she graduated Summa Cum Laude with a degree in Sociology and South Asian Studies.
Dr. Parikh is extremely invested in the well-being of her patients, and uses her extensive medical, sociological and psychological training to provide the most comprehensive and compassionate care for the people she treats. She supplements her biologic conceptualization of mental illness with her deep understanding of psychoanalytic thought, which enables her to think holistically about the human experience and the pathologies that may arise.
Dr. Parikh is also highly involved in both local and international community service projects. She is currently on the Editorial Board for Institutionalized Children: Explorations and Beyond, an international journal that provides a forum for discussion of the mental and physical care of orphan children in developing South Asian countries. Over the last decade, she has also fundraised extensively and volunteered internationally through Home of Hope, Inc. a U.S. based nonprofit charity that aids orphans and disadvantaged children across the world. Finally, she is an avid editorial writer for local newspapers through Savant Care.
Affiliations & Accolades:
-
Editorial Board for Institutionalized Children: Explorations and Beyond (Journal)
-
Best of Los Altos 2016 (Psychiatrist category)
-
Best of Los Altos 2015 (Psychiatrist category)
-
Fellowship, San Francisco Center for Psychoanalysis
-
Summa Cum Laude, UC San Diego (Sociology, South Asian Studies)
Vikas Kedia -- CEO/CTO and Co-Founder of Savant Care; Founder & CEO, InterNext Technologies; Founder & CEO, Securities Performance Algorithms
After graduating from the Indian Institute of Management in Bangalore, India, Vikas turned down a $100,000 job offer to become an entrepreneur.
In 2000, Vikas became the first Indian to be named one of the 20 finalists of Stanford University’s prestigious Olympics of Business Plans. As a graduate student at Stanford, he dazzled Professor Alex Aiken, Tencent Chair of Computer Science, by becoming the fastest compiler in his class.
In 2003, Vikas founded InterNext Technologies, Inc., composed of his 4 online finance communities whose collective membership exceeds half a million users. He served as InterNext CEO and Technology Architect, deploying load-balanced systems with failover capabilities over clusters of Linux-based web servers, database servers, mail servers, and asterisk based VOIP soft switches. He also deployed IPKVM, IPMI, remote rebooter switches, and HP Procurve switches, and built Supermicro servers.
Vikas served as System Administrator for Oak View Law Group, APC in Palo Alto, CA for 4 years, where he maintained an uptime of 99.99% and managed 200 Xen containers running LAMP, Asterisk, and memcache. He established a system of in-house base load servicing while exporting excess load to the cloud, saving the firm over $200,000 per year.
In 2011, Vikas founded Securities Performance Algorithms, a fintech firm that provides buy and sell quotes, risk management infrastructure, and other efficiencies to securities investors.
In 2012, Vikas co-founded Savant Care with Dr. Savant and Dr. Parikh. In his dual role as CEO and CTO, he led a team of 15 programmers to create Electronic Medical Record (EMR) software featuring a conversational UI.
**Accolades: **
-
National Merit Scholarship from the Government of India
-
Certificate of Merit from the Government of India
**Skills: **
-
C / C++ / Python (Advanced)
-
Linux, AWS, Mysql, Nginx (Advanced)
Healthchain has a business model that benefits patients, doctors, pharmacies, researchers, and eventually also insurance companies and other market participants. Software for most of this is already developed, and the only thing missing is users.
No competitor we've reviewed has a similarly inclusive roadmap -- let alone one for which it is already so well-prepared. Some competitors have working products, but their approach is isolated from the rest of the healthcare ecosystem and will fail when they are unable to make a strong business case for adoption by other market participants. For example, with only 1000 prescriptions on Healthchain in a given zipcode, pharmacies will see their profit margins increase substantially. This could happen in 2018 with Healthchain, or 2020 -- maybe -- with a competitor like MediBloc (http://medibloc.org/en).
Below is a detailed summary of our competitive advantage with respect to a few others:
-
Medicalchain does not offer many of the market efficiencies that Healthchain does (pharmacy bidding, etc.).
-
Medicalchain says it will offer tokens to doctors to encourage participation. This solution drastically underestimates the reluctance of doctors to change their routines and learn new software. Healthchain knows from experience that even free access to a world-class EMR, which otherwise costs doctors hundreds of dollars per month, is rarely enough to convince doctors to switch to new software. Medicalchain only offers doctors tokens, which assumes a deep and unrealistic doctor trust in a brand new cryptocurrency. By contrast, Healthchain offers doctors the opportunity to attract new patients for free (a service for which ZocDoc charges $300/month) without asking doctors to change their routine at all.
-
Medicalchain does not account for how to compete with existing EMR software companies and industry incentive structures. As has been seen in many industries, merely having a superior system far from guarantees its displacement of the current one.
-
Medicalchain is far behind Healthchain on software development. Many of the functions Medicalchain will offer in 2018 are already possible using Healthchain software, including many that Medicalchain has no plans to offer (e.g., pharmacy bidding system, EMR for doctors, decentralized token foundation, etc.)
- MediBloc does not have a personal medical record or an electronic medical record on blockchain. MediBloc aims to create a platform that will allow app development on the blockchain. Their roadmap indicates that the platform will be released to developers in December 2018.
Healthchain currently offers the very sort of apps MediBloc hopes to enable starting one year from now. Personal medical records (PMR) to store patient data and electronic medical records (EMR) to help doctors organize patient files are the primary software tools of the healthcare industry, and Healthchain has already developed and deployed these on blockchain. Healthchain's EMR was developed over 3 years with input from 15 doctors. Healthchain is therefore 1-4 years ahead of MediBloc in terms of software development.
- MediBloc does not aim to create the market efficiencies that we do. For example, Healthchain allowing pharmacies to bid on patient prescriptions will lower medical costs for patients and increase profit margins for pharmacies. These benefits not only provide greater value for both patients and pharmacies, but present a clear business case for pharmacy adoption. Insurance companies, which benefit from lower prescription payouts, are also incentivized to support Healthchain adoption.
Doc.ai is a likely partner. Doc.ai focuses on drawing insights from data, rather than creating market efficiencies based on patient-owned data. We are currently in talks with the founders of Doc.ai, Walter and Sam DeBrouwer, to see how we might work together to offer patients greater value for their data.